The morning sun glinted off the wet sidewalks as Thomas wiped his hands on a ragged towel, surveying the small engine in front of him. Retirement hadn’t dulled his love for fixing things — lawnmowers, old trucks, even his neighbor’s snowblower — he liked to keep busy, stay useful.
Today, though, a slow, gnawing pain brewed deep in his belly, pulling at him like a stubborn hand refusing to let go.
“Must’ve pulled something,” he muttered, brushing it off. He reached again for his wrench, but this time, the pain surged outward, a dull pressure spreading into his lower back. He straightened, grimacing, sweat breaking out on his forehead despite the cool autumn air.
His wife, Martha, called from the porch. "Tommy, you all right?"
He hesitated. Admitting weakness was foreign to him — but as he pressed his hand against his abdomen, he felt something strange. A pulsing mass, firm yet tender, like something alive just under the surface.
He forced a grin. "Just a cramp," he lied.
But deep down, Thomas knew something wasn’t right.
The pain worsened overnight. It was a deep, relentless ache, worse when he stood, mildly better when he lay flat. By morning, Thomas could no longer ignore it. At Martha’s insistence, they drove to the emergency department.
The fluorescent lights buzzed overhead as he sat hunched in triage, one hand instinctively resting on his lower abdomen.
A young nurse approached. "OK, Mr. Sullivan, I see you are 71 years old, can you tell me what brings you in today?"
Thomas shifted uncomfortably. “Got this pain in my belly. Been there since yesterday. Feels... weird. And there’s this bump. It's pulsing.”
The nurse's expression sharpened. She palpated gently, her fingers freezing mid-press. Without breaking composure, she stood up.
"Let's get you seen right away.
Minutes later, in the exam room, Dr. Husain entered, introducing himself warmly. He knelt to Thomas's eye level, listening carefully as he described the slow progression of pain, the backache, the odd sensation of pressure.
"No trauma? No fevers? No blood in the stool or urine?" he clarified.
Thomas shook his head. His medical history was notable only for hypertension, diagnosed fifteen years ago but poorly controlled ("I don't like taking pills," he'd confessed sheepishly).
Dr. Husain leaned over and gently palpated his abdomen. His hand paused at the midline, just above the navel.
There it was — a pulsatile mass, undeniable, ominous.
His mind clicked through differentials: abdominal aortic aneurysm, retroperitoneal mass, mesenteric tumor — but the most urgent worry was clear.
He ordered a bedside ultrasound immediately.
As Thomas lay back, the ultrasound technician smeared cold gel across his abdomen.
On the black-and-white screen, the abdominal aorta loomed into view — and widened dramatically at the level of the bifurcation.
Normally, the aorta measures about 2 cm in diameter.
Thomas’s measured 5.8 cm, with a thin, irregular wall — a ticking bomb inside his belly.

An abdominal aortic aneurysm (AAA) forms when the wall of the aorta, weakened by years of hypertension, smoking, or genetic predisposition, begins to bulge outward under pressure.
The collagen and elastin that normally keep the vessel strong fray and disintegrate, allowing the artery to expand like a worn-out tire.
If the aneurysm grows too large — typically over 5.5 cm — the risk of rupture soars, and rupture often means sudden, catastrophic death.
Dr. Husain’s heart quickened. This wasn’t just a finding — it was an emergency waiting to happen.
He returned to Thomas and Martha, his voice steady.
"Mr. Sullivan, we found a large bulge in the main artery in your abdomen — something called an abdominal aortic aneurysm. It's quite sizeable, and it could rupture if left untreated."
Martha’s face paled. "Rupture? What does that mean?"
"If it tears, it can cause massive internal bleeding very quickly. It's life-threatening. We need vascular surgery to evaluate you right away."
Thomas looked stunned. "But... I was just working on my tools yesterday."
Dr. Husain nodded. "It often doesn’t cause symptoms until it gets big or leaks. You didn’t do anything wrong — we just need to act now."
"We are taking you for a CT scan right now," said Dr. Husain as he quickly assisted in transporting Thomas to Radiology.
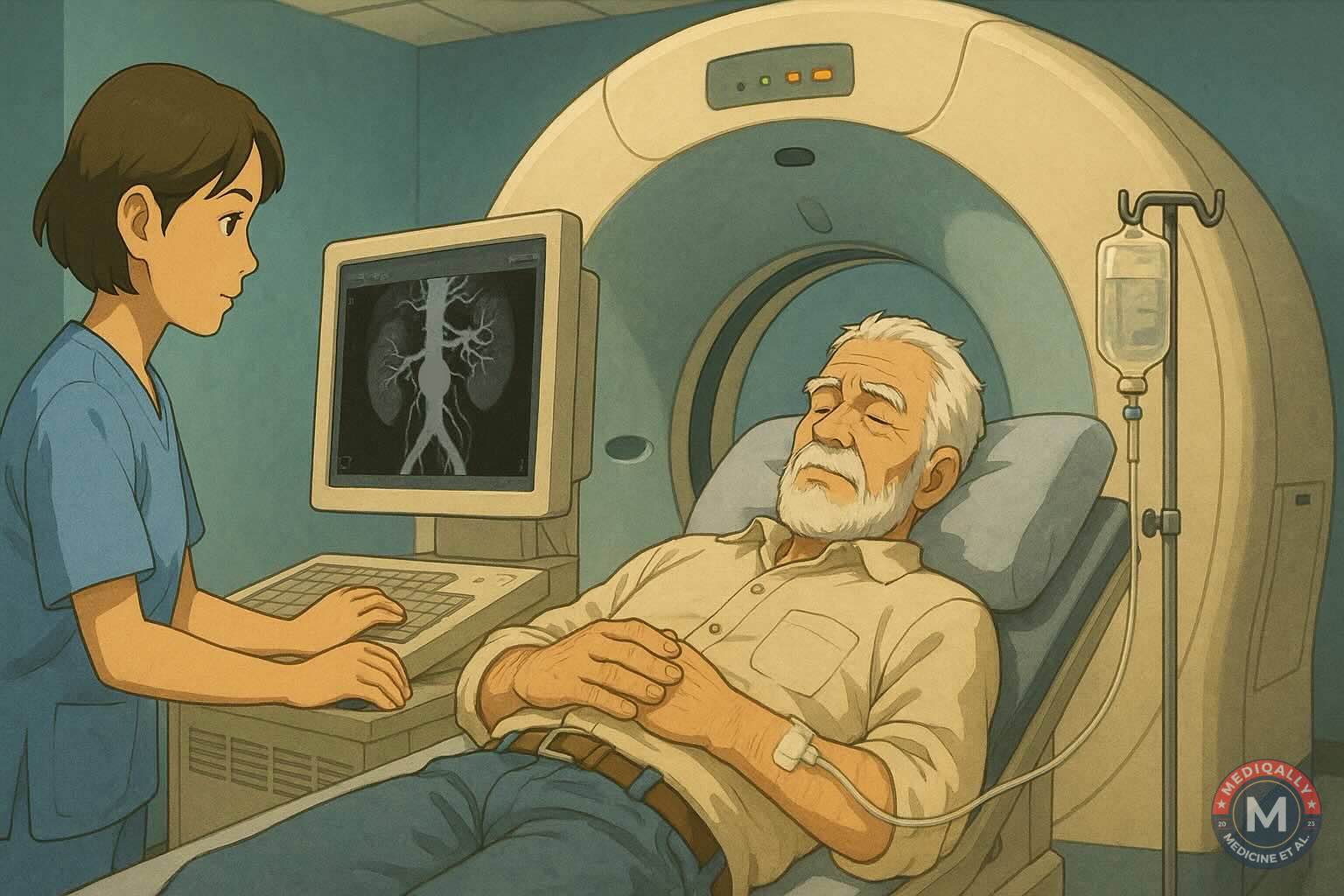
A stat CT angiogram confirmed the findings:
- Juxtaarenal AAA
- 5.8 cm diameter
- No active leak or rupture yet
- No evidence of involvement of renal arteries

Vascular surgery was paged, and within the hour, Dr. Rowe, the vascular surgeon, stood at his bedside.
"We have two options," Dr. Rowe explained.
"Open surgery, where we replace the damaged portion of the aorta with a graft. Or endovascular repair — a stent placed through small incisions in your groin."
Given Thomas’s anatomy and relative stability, endovascular aneurysm repair (EVAR) was a possibility.
After discussing risks and benefits — bleeding, graft migration, infection — Thomas chose EVAR.
By evening, he was on the operating table.
The surgery went smoothly, a thin metallic stent now bridging the vulnerable segment of Thomas’s aorta. In the recovery room, Martha held his hand tightly, tears streaming down her face.
"I thought I was going to lose you," she whispered.
Thomas squeezed back, words failing him.
Later that night, Dr. Husain sat at his desk, thinking about how easily Thomas could have died — how many patients never made it to the hospital in time.
He wondered how many silent aneurysms lurked undetected, waiting to rupture.
Screening for AAA isn’t routine for everyone — only for certain high-risk groups:
- Men aged 65–75 who have ever smoked
- Patients with family history
Thomas had never been screened.
Would things have been different if someone had caught it earlier?
Thomas spent three days in the hospital.
He learned how to monitor his blood pressure carefully, to take his medications faithfully, and to come back for regular imaging to check the graft.
Everything felt sharper now — the smell of rain on concrete, the rustle of leaves, the soft murmur of nurses' voices.
Life, he realized, was far more fragile than he had believed.
Key Clinical Takeaways
- Abdominal aortic aneurysms (AAA) are often asymptomatic until they reach a critical size or rupture.
- Risk factors include smoking, hypertension, male sex, age >65, and family history.
- A pulsatile abdominal mass and deep abdominal/back pain in a high-risk patient should raise immediate suspicion for AAA.
- Ultrasound is the first-line screening and diagnostic tool; CT angiography is essential for surgical planning.
- EVAR offers a less invasive alternative to open repair but requires careful anatomical evaluation and lifelong surveillance.


Member comments